The five pillars of cancer care currently comprise surgery, radiotherapy, traditional chemotherapy, precision therapy, and immunotherapy. Each of these treatments addresses cancer in different ways, targeting the malignancy itself. However, the link between obesity and cancer has been well established, and obesity has been recognized as a risk factor for certain types of cancer. Given the strong correlation between obesity and cancer risk, including potential molecular mechanisms that may foster cancer growth, an emphasis on weight management could represent a profound shift in cancer prevention and treatment.
The integration of obesity management into the treatment paradigm could involve a multidisciplinary approach, incorporating dietary interventions, physical activity, behavioral changes, and potentially even novel pharmacological agents aimed at curbing weight gain. By addressing obesity as a modifiable risk factor, healthcare professionals may be able to not only treat cancer more effectively but also prevent it in certain instances. The introduction of weight management as another pillar in cancer care would require rigorous scientific research and clinical trials. However, if successfully implemented, it could revolutionize the way we approach cancer treatment and prevention, placing a strong emphasis on the patient’s overall well-being and lifestyle choices, and ushering in a new era of holistic cancer care.
It is the purpose of this website to draw attention to this unmet need in medicine and to address some of the questions that surround this new medical field.
AI Generated Summary Podcast (8:02)
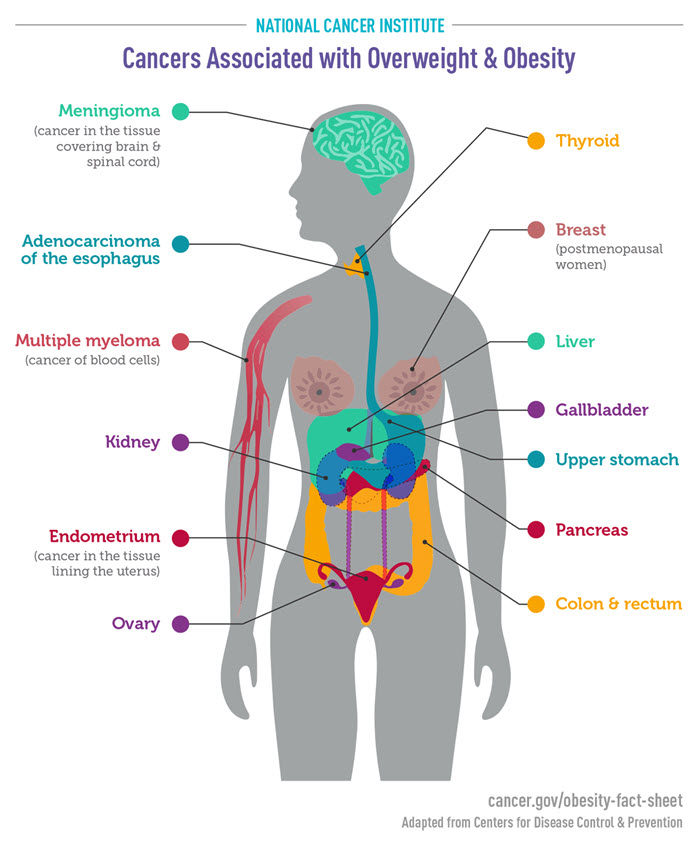
NCI Obesity Fact Sheet
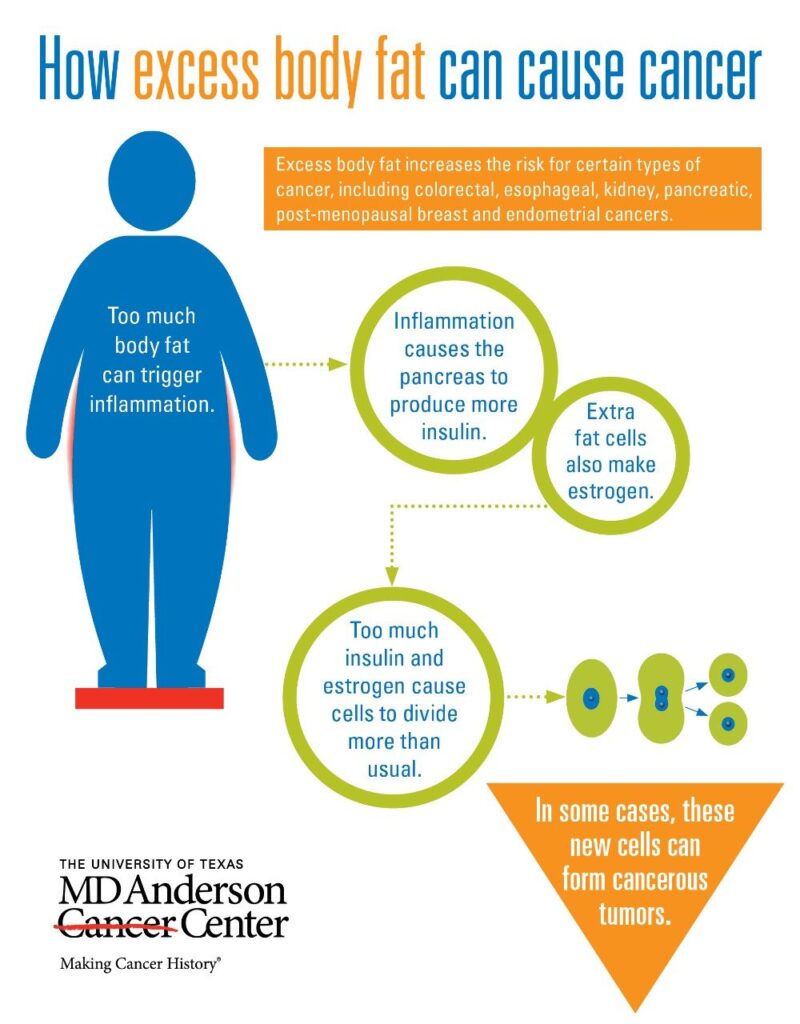
Obesity is a major health concern that is not only associated with chronic diseases like cardiovascular disease, but it is also linked with an increased risk of cancer. According to the National Institutes of Health (NIH), 4-8% of all cancers can be attributed to obesity. The underlying mechanism of obesity causing cancer is complex, and researchers are still trying to gain a better understanding of it. However, researchers know that certain lifestyle changes can help reduce the risk of developing cancer due to obesity. In particular, diet, exercise, and behavior therapy are the mainstay of intervention to fight against obesity and, thereby, lower the risk of cancer. For more information, please click on the link to the research paper cited and also check out the NIH’s National Cancer Institute infographic on the cancers associated with overweight and obesity.
AI Generated Summary Podcast (9:48)
This webpage from the Centers for Disease Control and Prevention (CDC) explores the strong link between obesity and cancer risk. It outlines how being overweight or obese increases the likelihood of developing 13 specific types of cancer, which account for 40% of all cancer diagnoses in the United States. The article also discusses how excess weight can lead to bodily changes, such as inflammation and hormone imbalances, which contribute to cancer development. Finally, the CDC provides practical steps for individuals and healthcare providers to reduce the risk of obesity-related cancers, emphasizing the importance of healthy lifestyle choices and preventative measures.
AI Generated Summary Podcast (7:06)
Summary
The World Health Organization (WHO) has released a report on the growing epidemic of obesity in Europe and Central Asia. The report reveals that obesity is a major cause of preventable death and disability, linked to 13 types of cancer, and is expected to surpass smoking as the leading preventable cancer risk factor in some countries. The report emphasizes that obesity is a complex condition that requires multidisciplinary treatment and management, and urges the implementation of comprehensive policy interventions, such as restricting unhealthy food marketing to children, taxing sugar-sweetened beverages, and improving health systems to address obesity management.
AI Generated Summary Podcast (18:57)
Summary
This Cancer Research UK excerpt details the strong link between obesity and cancer risk in adults. Obesity is identified as the second leading cause of cancer in the UK, increasing the likelihood of developing 13 specific cancer types. The text explains how excess fat influences growth hormones, inflammation, and sex hormones, thereby promoting cellular division and cancer development. Methods for assessing healthy weight, such as BMI and waist-to-height ratio, are discussed, along with advice on maintaining a healthy weight to reduce cancer risk. Importantly, the text clarifies that obesity does not cause cancer in children.
AI Generated Summary Podcast (13:24)
Summary
This paper proposes a new model of obesity that combines the obesogens model (OBS) and the oxidation-reduction model (REDOX). The OBS model posits that environmental chemicals can disrupt hormonal signaling and lead to adiposity, while the REDOX model suggests that reactive oxygen species (ROS) generated by these chemicals can alter metabolic signaling, increasing insulin secretion and disrupting energy efficiency. The authors argue that this OBS/REDOX model can explain the data supporting both the energy balance model (EBM) and the carbohydrate-insulin model (CIM), which are the two most prevalent models of obesity. They propose that obesogens act by interfering with hormone receptors and hijacking redox signaling pathways, ultimately leading to inappropriate and false signals about energy status, resulting in weight gain.
AI Generated Summary Podcast (10:11)
Summary
This research paper investigates the “obesogenic memory” – the persistent cellular and epigenetic changes in adipose tissue after weight loss. Using single-nucleus RNA sequencing and multi-omics analysis in both humans and mice, the study demonstrates that significant transcriptional and epigenetic alterations remain in adipocytes even after substantial weight loss. These persistent changes, primarily driven by epigenetic modifications at enhancers and promoters, prime cells for pathological responses, potentially explaining the common “yo-yo” effect of weight regain. The findings suggest that targeting these epigenetic changes could improve long-term weight management.
AI Generated Summary Podcast (17:39)
Summary
This research review examines the complex relationship between obesity and cancer risk. It details several mechanisms linking obesity to cancer development, including chronic inflammation, hormonal imbalances (especially estrogen and progesterone), gut microbiota dysbiosis, and adipokine dysregulation. The review also explores various prevention strategies, such as lifestyle changes, weight-loss medications, and bariatric surgery, and proposes areas for future research, focusing on the distinctions between hereditary and acquired obesity, the impact of aging, and the interplay between obesity, gut microbiota, and cancer progression. Ultimately, the authors aim to provide a foundation for developing more effective and personalized cancer prevention strategies for obese individuals.
AI Generated Summary Podcast (20:50)
Summary
This research article from JAMA Psychiatry reports on a large-scale Swedish cohort study investigating the effects of GLP-1 agonists, specifically semaglutide and liraglutide, on alcohol use disorder (AUD). The study found a significantly reduced risk of AUD-related hospitalizations among users compared to non-use periods, surpassing the effectiveness of standard AUD medications. These findings suggest a potential new treatment avenue for AUD, though further randomized clinical trials are needed to confirm causality. The study leveraged nationwide Swedish registries to track patient data and employed a within-individual analysis design. The results highlight semaglutide and liraglutide as promising candidates for AUD treatment.
AI Generated Summary Podcast (11:13)
Summary
This article, published in the New England Journal of Medicine, reports on the SUMMIT trial, a randomized, placebo-controlled study investigating the effects of tirzepatide, a weight-loss drug, on cardiovascular outcomes in obese patients with heart failure and preserved ejection fraction. The trial showed that tirzepatide significantly reduced the risk of death from cardiovascular causes or worsening heart failure compared to placebo. Furthermore, tirzepatide improved patients’ quality of life and exercise capacity. Adverse events, primarily gastrointestinal, were reported, but were generally manageable. The findings suggest tirzepatide may offer a beneficial treatment option for this patient population.
AI Generated Summary Podcast (20:37)
Summary
This systematic review assesses the effectiveness and safety of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) for weight loss in adults without diabetes. The analysis included 26 randomized controlled trials with over 15,000 participants, examining various GLP-1 RAs and co-agonists. Results indicated that these agents, particularly tirzepatide, semaglutide, and retatrutide, led to significant weight loss compared to placebo. While adverse events, mainly gastrointestinal issues, were common, serious events were rare. The study concludes that GLP-1 RAs are effective for weight loss in non-diabetic adults with overweight or obesity, with manageable safety concerns. These medications also showed benefits in reducing BMI, waist circumference, and blood pressure.
AI Generated Summary Podcast (15:58)
Summary
This research uses U.S. Department of Veterans Affairs data to comprehensively assess the effects of glucagon-like peptide-1 receptor agonists (GLP-1RAs) on 175 health outcomes in individuals with diabetes. By comparing GLP-1RA use to several control groups (sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors, and usual care), the study maps both the benefits (reduced risks of various disorders) and harms (increased risks of other conditions) associated with GLP-1RA treatment. The findings reveal broad pleiotropic effects, impacting areas such as neuropsychiatric health, cardiovascular health, renal function, and the risk of infections. These results, while based on a large cohort, acknowledge limitations concerning generalizability due to the sample’s demographics. The study concludes by recommending further research to explore the potential of GLP-1RAs in treating various conditions and to better understand their effects.
AI Generated Summary Podcast (17:31)
Summary
This study explores the potential of semaglutide, a glucagon-like peptide 1 receptor agonist (GLP-1RA), as a treatment for alcohol use disorder (AUD). A randomized clinical trial assessed semaglutide’s impact on alcohol consumption and craving in adults with AUD. The results indicated that low-dose semaglutide reduced alcohol consumption during laboratory self-administration tasks and decreased weekly alcohol craving. While it didn’t significantly alter all measures of weekly consumption, the study showed promise in reducing drinks per drinking day and heavy drinking episodes. These findings suggest that GLP-1RAs, like semaglutide, merit further investigation as a possible therapeutic intervention for AUD, especially considering their increasing use for other conditions like diabetes and obesity. The research also noted a potential for reducing cigarette consumption in smokers, highlighting a possible dual benefit.
AI Generated Summary Podcast (16:21)
Summary
This research paper details the Breast Cancer Weight Loss (BWEL) trial, a large-scale, randomized controlled trial investigating whether weight loss interventions can improve outcomes for overweight or obese women with breast cancer. The study uses a two-year, telephone-based lifestyle intervention incorporating dietary modifications, increased physical activity, and behavioral strategies, drawing upon elements from successful prior trials like the Diabetes Prevention Program and Look AHEAD. The intervention’s primary goal is a 10% weight loss, delivered via 42 coaching sessions, with flexibility to meet diverse participant needs. Researchers aim to determine if weight loss impacts invasive disease-free survival and overall survival, potentially influencing future breast cancer treatment.
AI Generated Summary Podcast (15:09)
The connection between a new class of weight loss drugs and cancer risk reduction – MSKCC
Memorial Sloan Kettering Cancer Center shared a post on X:
“In this episode of Cancer Straight Talk, Diane Reidy-Lagunes sits down with MSK’s Neil Iyengar to discuss the intriguing connection between a new class of weight loss drugs, called GLP-1 agonists, and cancer risk reduction.
Obesity is associated with significantly increased risk of more than 20 chronic diseases and health conditions that cause devastating consequences and increased mortality. Beyond the significant personal toll of obesity, related health complications are driving up health care costs and threatening employers’ bottom lines.
Obesity is a complex chronic disease in which abnormal or excessive accumulation of body fat impairs health. Adult and adolescent obesity rates have more than doubled since the 1980s — in the U.S. today, obesity affects over 42% of adults and 20% of 12-19 year olds. Obesity and its related complications are major drivers of rising healthcare costs, diminished health-related quality of life, and the recent decline in U.S. life expectancy.
These downloadable STOP Fast Fact sheets are designed to provide basic information about the science of obesity and current strategies to address it.
Obesity-Related Chronic Disease
Obesity and AI/AN Populations
Obesity and COVID-19
Mental Health and Obesity
Adolescent Obesity
Obesity and Cancer
Benefits of Weight Loss
Racial Disparities and Obesity
COVID-19, Food Systems, and Obesity
Obesity in the Workplace
Obesity in Early Life
Obesity Care Coverage
Trends in Obesity Prevalence
Costs of Obesity
Weight Bias and Stigma
Causes of Obesity
Health Care Providers and Obesity Care
Obesity-Related Chronic Disease
The Battle of the Incretins is ON!
AI GENERATED SUMMARY PODCAST (13:12)
Summary
The Link Between Obesity and Cancer provides a comprehensive and up-to-date review of the relationship between obesity and cancer. It opens with a global perspective on obesity and cancer incidence, followed by in-depth discussions on cancers for which we have sufficient and new evidence of a causal relationship with obesity. Readers will gain fundamental knowledge about which different cancer types are related to obesity and why. The book provides a significant knowledge base for clinicians to know when to act, along with specific management guidelines for patients with obesity as well as how to understand the potential risk factors and how to directly or indirectly minimize these risks. The book also provides scientific data for any researcher in the field, identifying the molecular mechanisms and links behind the development of malignancy and promoting research on new affective target pathways m developing therapeutic strategies.
Key Features
• Provides essential knowledge on how to understand the link between obesity and cancer and why and how this occurs; enables readers to gain fundamental knowledge on which cancer types are related to obesity and why
• Provides a significent knowledge base for clinicians on when to act, along with patient management guidelines for patients with obesity as well as how to understand potential risk factors and how to minimize them
• Contains new scientific data and findings for researchers, which identify the molecular mechanisms and links behind the development of malignancy
The book, The Link Between Obesity and Cancer is on sale at Amazon or at ScienceDirect®.
Summary
AI Generated Summary Podcast (7:52)
Kallyope eyes clinic with K-554 for obesity
Kallyope Inc. has outlined plans to initiate phase I studies this year with K-554, a non-incretin peptide candidate offering a new mechanism of action in obesity.

STAT+: Eli Lilly’s Zepbound, on top of immunology drug, helped reduce psoriatic arthritis symptoms
Eli Lilly said Thursday that adding its weight loss drug Zepbound on top of its immunology therapy Taltz helped obese patients with an autoimmune condition that causes joint pain more than Taltz did alone. The

7 CES 2026 technologies that made science fiction feel uncomfortably practical
CES 2026 had no shortage of AI products, but a quieter pattern stood out across booths that had little else in common. Some of the most attention-grabbing technologies weren’t built for screens or productivity dashboards.

New Lilly data suggest Zepbound boosted effect of autoimmune drug
New Phase 3b data from Eli Lilly suggest that its blockbuster weight loss drug helped boost the efficacy of an autoimmune treatment in select patients with active psoriatic arthritis who were overweight or obese. …
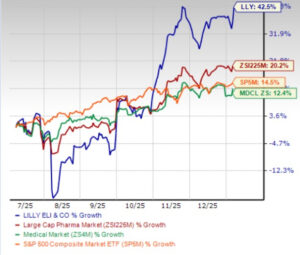
Is LLY’s Ventyx Deal Another Attempt at Diversification Beyond GLP-1?
Eli Lilly LLY has pursued a series of acquisitions since early 2025 to strengthen its pipeline and support long-term growth amid intensifying competition in the obesity space. While cardiometabolic health remains its core focus, LLY is

Former GLP-1 users regain lost weight after about 18 months, study says – The Washington Post
Former GLP-1 users regain lost weight after about 18 months, study says The Washington Post People Who Stop Taking Weight-Loss Medications Regain Weight Within 2 Years, Study Says People.com Less than two years after stopping obesity drugs,

The 20 most influential drug approvals of 2025: GoodRx
GoodRx has named 20 medications and vaccines as the most influential FDA approvals of 2025, spotlighting first-in-class drugs, new indications, and therapies with the potential to significantly affect public health. 1. Nereus (tradipitant) for motion
GLP-1 Market Trends and Global Forecasts 2025-2035: 150+ Candidates Intended for the Treatment of Multiple Indications, are Currently Either Approved or Being Investigated – ResearchAndMarkets.com
DUBLIN–(BUSINESS WIRE)–The “GLP-1 Market: Industry Trends and Global Forecasts, Till 2035” report has been added to ResearchAndMarkets.com’s offering. The global GLP-1 market is estimated to grow from USD 62.2 billion in the current year to