Lilly’s Lower-Cost Zepbound Options Could Ease Patient Transition From Compounded GLP-1s
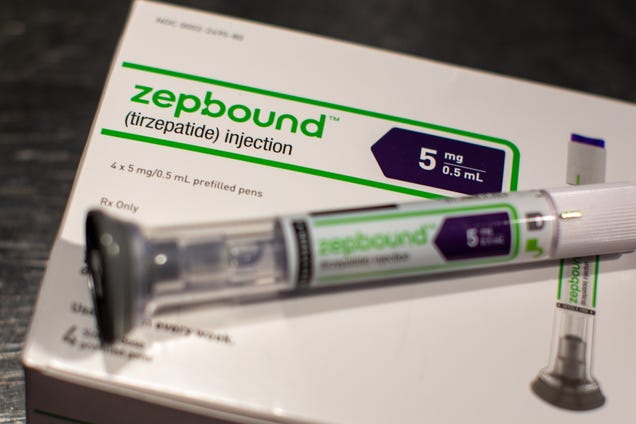
The Zepbound line extension and price reductions are aimed to appeal to self-pay customers. (Shutterstock). Eli Lilly is introducing reduced price …
GLP-1 Therapies and Cardiovascular Health: Unanswered Questions and Future Directions
Are GLP-1 therapies truly safe for long-term cardiovascular health? Dr Pandey unpacks key gaps in current research, real-world data, …
Doctors using GLP1 to help with knee replacement surgery – WPBF
A local surgeon finds GLP 1 helps his patients who need knee and hip replacements.
ASBM: With GLP-1 Shortage Over, Increased Focus on Safe Compounding is Needed
… of the shortage for popular GLP-1 weight loss drugs Ozempic and Wegovy, the Alliance for Safe Biologic …
Obesity late-comer AbbVie teams up with Gubra | The Pharmaletter

In a partnership marking AbbVie’s entrance into the weight management field, the US pharma major has signed a licensing deal with Denmark’s Gubra …
AbbVie Ventures Into Obesity Treatment Market with $2.2 Billion Gubra Deal – IndexBox

… Zepbound, which are based on the GLP-1 hormone. This differentiation could provide AbbVie with a unique foothold in the competitive landscape. On …
Cancer? No, thank goodness, it’s just high cholesterol. – Harvard Gazette
… GLP-1.” “Our population is getting healthier. You don’t have to be a full-fledged diabetic with heart failure, or risk, to benefit from GLP-1.
Why The Next Big Thing Might Not Be, After All – IFT.org
Arlin Wasserman questions the viewpoint that GLP-1 drugs will have a major impact on the food industry.
GLP-1s: The Next Wave of Weight Loss – IFT.org
Food manufacturers are responding to the growing popularity of GLP-1 drugs with product innovations designed to support consumers in their weight …
Novel antibody could help prevent bone, muscle loss due to GLP-1 drugs

Post Content
